This news might hold the attention of cancer patients. A research claims that Helicobacter pylori, the only bacterium recognized to live in the inhospitable setting of the human stomach apparently triggers an enzyme in host cells directly. This has supposedly been linked to numerous kinds of cancer, counting gastric cancer.
Chronic infection with H. pylori is said to be a well-documented threat issue for various kinds of gastric cancer. But scientists have apparently not yet found out the means by which detailed bacterial factors add to cancer growth. This research is alleged to be the first to exhibit that a factor generated by the bacterium directly may generate poly (ADP-ribose) polymerase-1 (PARP-1), an enzyme discovered principally in the nucleus of animal cells. PARP-1 is said to be a controller of the host’s inflammatory response and host cell death, both of which are claimed to be trademarks of H. pylori infection.
PARP-1 is apparently best known as a standard element of the cellular machinery that impairs injured DNA. But in specific kinds of cancer, this enzyme may really improve tumor survival and weaken chemotherapies intended to harm DNA in cancer cells. A new human clinical trial is believed to have discovered that drugs that inhibited PARP-1 apparently decreased tumor development in breast-cancer patients with mutations in particular DNA-repair (BRCA-1 and BRCA-2) genes. BRCA-1 mutations supposedly also are linked to an augmented threat of stomach cancer.
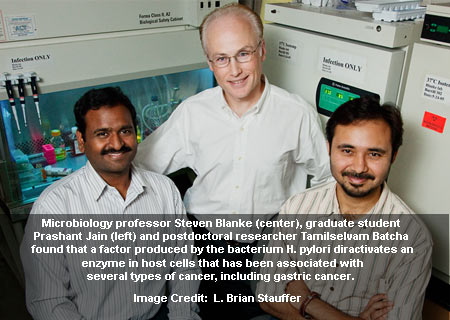
The recent research apparently dealt with the most pressing health issue connected to H. pylori infection. This was mentioned by Steven Blanke, a University of Illinois professor in the department of microbiology and Institute for Genomic Biology and principal investigator on the research.
Blanke and his graduate student Carlos Nossa formerly had illustrated that a protein factor discharged by H. pylori apparently alters an unrevealed host protein in a method steady with an enzymatic reaction called ADP-ribosylation. Other bacterial toxins, counting cholera toxin and diphtheria toxin ‘ADP-ribosylate’ is said to host proteins in ways that may augment the survival or broadcast of the bacteria that generate them.
ADP-ribosylation may supposedly be trailed by integrating a radio-isotope of phosphorous i.e. 32P into a small molecule that is needed for the result. During ADP-ribosylation, H. pylori are thought to relocate the 32P from the labeled molecule to a host protein, thus classifying it with a radioactive fingerprint. Additional analysis apparently exposed that the radio-labeled host protein was PARP-1.
At this point, the team was of the opinion that the bacterium was ADP-ribosylating PARP-1. But when they hereditarily modified the useful areas of PARP-1, they fully obstructed the H. pylori-dependent change. As PARP-1 also has poly-ADP-ribosylation enzymatic activity, which is essential for its authoritarian and DNA-repair role in cells, the team comprehended that something in the H. pylori arsenal was apparently triggering the PARP-1 enzymatic activity directly, rather than ADP-ribosylating.
Supplementary researches apparently corroborated that H. pylori certainly generated PARP-1 during infection of human gastric cells.
Blanke commented, “These studies potentially provide a direct molecular link between H. pylori infection and the activation of a factor known to be involved in the survival of cancerous cells. Although PARP-1 can potentially be activated indirectly as a host cell response to some infections, this is the first example of a bacterium that can activate PARP-1 directly, perhaps in this case as a mechanism for H. pylori to promote inflammation and/or the death of host cells during long-term infection.â€
The researchers are conducting more experiments to discover the bacterial factor that triggers PARP-1. This could be a promising objective for drugs to treat or avert the issues related to lasting infection with H. pylori.
The research was published in the National Academy of Sciences.