Umbilical cord blood cells could effectively be reprogrammed to work like embryonic stem cells, setting the foundation for the formation of a complete collection of tissue-matched, cord blood-derived induced pluripotent stem (iPS) cells for off-the-shelf applications. This was claimed by a research at the Salk Institute for Biological Studies and the Center for Regenerative Medicine in Barcelona, Spain.
Due to their early origin, around more than 400,000 cord blood units are apparently stored along with immunological information. Due to their early origin, cells in umbilical cord blood may comprise of a negligible amount of somatic mutations and could acquire the immunological immaturity of newborn cells, letting the HLA donor-recipient equivalent to be less than ideal without the danger of immune rejection of the transplant.
“Cord blood stem cells could serve as a safe, “ready-to-use” source for the generation of iPS cells, since they are easily accessible, immunologically immature and quick to return to an embryonic stem cell-like state,†commented,Juan-Carlos Izpisua Belmonte, Ph.D., a professor in the Salk’s Gene Expression Laboratory.
To match patients and donors for bone marrow or cord blood transplants, Human leukocyte antigen (HLA) typing is used. It is said to be an exceptional surface marker which is apparently discovered on almost all the cells in the body and assists the immune system to differentiate between ‘self’ and ‘non-self’.
Izpisua Belmonte mentioned, “Selecting common HLA haplotypes from among already banked cord blood units to create iPS cell would significantly reduce the number of cell lines needed to provide a HLA match for a large percentage of the population.â€
The first adult cells were transformed into iPS cells. This may be an uncontroversial option to embryonic stem cells and a possible foundation for patient-specific stem cells. But to take a cell back in time is not only expensive but could also be complicated when those cells are supposedly required immediately to repair injured spinal cords or treat acute diseases, and it may not be viable when the effects of aging or chronic disease have permanently injured the collection of somatic cells.
Izpisua Belmonte remarked, “Patient-specific iPS lines have been advocated as a theoretically ideal clinical option to regenerate tissue but from a practical and cost-benefit aspect, this approach may not be feasible. Large scale production and banking of cord blood-derived iPS lines in a publically available network could be a viable alternative for future clinical applications.â€
Belmonte and his colleagues set out to convert hematopoietic stem cells which are cut off from cord blood into iPS cells. They not only effectively transformed them via two of the most frequently used factors i.e. OCT4 and SOX2 but they also did it in less time. The ensuing iPS cells were apparently identical to human embryonic stem cells.
Izpisúa Belmonte explained, “The population of cord blood cells used for reprogramming express reprogramming/stem cell factors at higher levels than those found in other adult somatic cells, which could explain why cord blood cells can be reprogrammed with less factors and in less time. It’s almost like they are already half-way there.â€
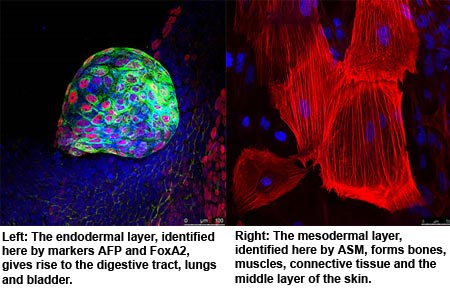
Moreover, the cord blood-derived iPS cells (CBiPS) apparently passed all usual examinations for pluripotency. This raised the stem cell tumors called as teratomas and distinguished them into derivatives of the three embryonic tissue layers, plus steadily beating cardiomyocytes and dopamine-producing neurons.
Izpisua Belmonte’s next objective is to influence cord blood cells to turn back time via techniques that may be considered harmless for clinical applications in humans. The original procedure for generating iPS cells, as well as the one used by Belmonte and his team, depend on the combination of foreign ‘reprogramming’ genes into the host-cell genome, a development that may be linked with risks counting mutation and the growth of cancers post iPS-cell transplantation, thereby limiting their therapeutic value.
Izpisúa Belmonte mentioned, “If we can show they also work for cord blood cells, this certainly could be a step forward towards the clinical application of iPS cells. We should focus our efforts on this particular cell source, CBiPS cells, at least in the near future.â€
Researchers are trying hard to develop alternative techniques that may let them reprogram cells without leaving any genetic traces, like exposing differentiated cells to tiny molecules.
This research was published in the journal Cell Stem Cell.