A Professor from the University of Central Florida Microbiology, Keith Ireton, has apparently exposed an earlier unidentified mechanism that may play a significant part in the spread of a fatal food-borne bacterium.
Listeria monocytogenes is a bacterium that may be the reason for pregnant women to lose their fetuses and could activate lethal cases of meningitis among the elderly or people with compromised immune systems. The bacterium has been associated with eruptions which may apparently be traced to food processing plants in the U.S. and Canada.
In 2002, there supposedly was a multi-state outbreak of listeriosis, which is claimed to be a grave disease caused by Listeria. It apparently resulted in about 46 confirmed cases, around seven deaths and roughly three stillbirths or miscarriages. Those cases in approximately eight states were apparently connected to people, who were consuming contaminated sliced turkey deli meat. There was another outbreak with about 142 cases of listeriosis from January to August 1985.
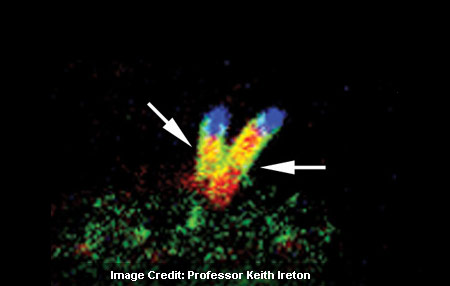
It has apparently been known long enough to find out that Listeria apparently spreads from one human cell to another. Bacteria apparently growing on one cell moves swift enough to form a finger-like structure that may stick out from the cell and may be pushed into an adjoining cell.
It has been found out by Ireton and colleagues that a formerly unfamiliar second process might assist in the spread of bacteria to healthy cells. The procedure may eventually overpower the second cell’s capability to protect itself from infection.
It appears as though the plasma membrane or outer layer of human cells may usually show signs of tension. To avert Listeria from scattering to adjacent uninfected cells, such tension might be anticipated. Nevertheless, Ireton’s lab discovered that a Listeria protein known as InlC seem to ease anxiety at the plasma membrane in infected cells. That may make it easier for moving the bacteria to distort the membrane and then may possibly extend into nearby, healthy cells.
Ireton’s laboratory may also account that the manner in which InlC reduces tension is by supposedly obstructing the job of a human protein known as Tuba. The usual function of Tuba in uninfected human cells seems to assist in generating tension at the plasma membrane. The Listeria protein InlC apparently inactivates Tuba, apparently decreases that tension and may allow bacteria to extend to nearby cells.
Ireton commented, “The idea that a pathogenic bacterium can spread by controlling membrane tension in the human cell has not been previously described in the scientific literature. Our discovery could have relevance for bacterial pathogens that cause Shigellosis or Rocky Mountain spotted fever, as these bacteria resemble Listeria in their ability to move inside the host cell and spread.”
Even though additional research may be required, Ireton mentioned that discovering this mechanism could help in potential therapies and may possibly open a window into understanding how some bacterial pathogens may cause disease.
This finding was published in the journal Nature Cell Biology.